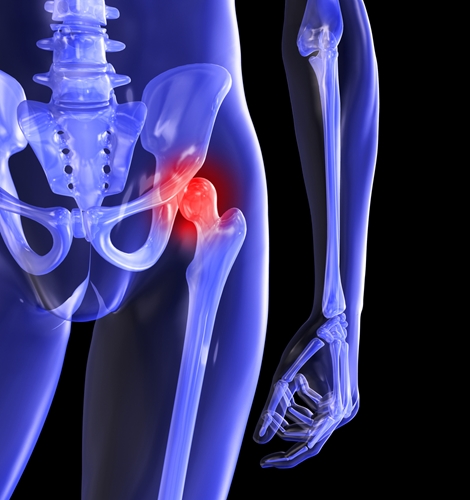
Study supports value of hip replacement among juvenile idiopathic arthritis patients
Although arthritis is typically associated with the aging process, different forms of the joint condition can affect young individuals. According to the National Institutes of Health, about 1 in every 1,000 children in the U.S. are living with juvenile idiopathic arthritis, totaling about 294,000 individuals altogether.
Some of these patients experience joint damage that is so severe that the best treatment is surgical replacement. However, it has not always been clear whether such approaches have much value for these individuals, particularly when they tend to be younger than other joint replacement patients and will likely need their prosthetics for a longer period of time.
One team of researchers from the Hospital for Special Surgery evaluated the outcomes of 56 individuals who underwent hip replacement procedures as treatment for juvenile idiopathic arthritis. They concluded that the operation is beneficial for patients younger than 35 years of age, as presented at the American College of Rheumatology annual meeting.
"Joint replacement can free patients from a life of unrelenting pain," Mark Figgie, M.D., senior author of the study and chief of the Surgical Arthritis Service at HSS, said in a statement. "It can enable those in a wheel chair to walk again. Patients can go back to school or work and get their lives back."
Implant survival is excellent
For their analysis, the study authors included individuals who underwent either bilateral or unilateral hip replacement surgery. The mean follow-up time was 12 years, and relevant data points included hip disability and osteoarthritis outcome scores, prosthetic survival time and self-reports on limitations of everyday activities.
Results showed that the implant survival rate among patients 10 years after surgery was 85 percent. After 20 years, that rate was 50 percent. Additionally, the data showed that implants tended to last longer among individuals who were first operated upon at 25 years of age or older, compared to patients who were younger at the time of the procedure.
Other results indicated that male patients reported better outcomes. Also, pain and limitations in everyday activity were worse among those who required customized prosthetics. The latter result did not surprise the researchers, who explained that customized prosthetics are usually required by patients whose disease tends to be especially severe.
Figgie and his colleagues emphasized that prosthetic survival times need to improve, especially in light of the fact that juvenile idiopathic arthritis patients have to live with the implants longer than older individuals do.
"The next step will be to evaluate which factors affect how long the implants last and work on improving implant design and durability," he said in his statement.
Orthopedic providers must keep up
Typically, hip replacement surgery is recommended in cases when conservative treatments do not produce any positive results. According to the National Institute of Arthritis and Musculoskeletal and Skin Diseases, these approaches include nonsteroidal anti-inflammatory medications, corticosteroids, biologic agents, disease-modifying antirheumatic drugs and physical therapy. Additionally, patients may want to look into alternative treatments, such as massage and acupuncture.
As orthopedic providers monitor the health of patients with juvenile idiopathic arthritis, it is important to remember that all health care professionals under the Health Information Protection and Portability Act need to transition to the 10th Revision of the International Classification of Diseases, or ICD-10, by Oct. 1, 2015. According to this system, the diagnosis coding under ICD-10-CM will contain between three and seven digits, instead of between three and five digits under ICD-9-CM. Meanwhile, ICD-10-PCS for inpatient procedure coding will be noted using seven alphanumeric characters.
When it comes to juvenile idiopathic arthritis, new orthopedic coding may be pertinent for disease state description, recommended treatment and patient progress.